Leukoplakia: Definition, Etiology, Clinical features, Classification, Histopathology, Investigations, Treatment, Malignant transformation and differential diagnosis
Definition:
Leukoplakia is a predominantly white patch or lesion of oral mucosa that can't be characterized as any other definable lesion. Some oral leukoplakia will transform into cancer.
Definable white lesions are:
1. Candidal leukoplakia
2. Hairy leukoplakia
3. Tobacco induced white lesions
4. Tobacco associated leukoplakia
5. Idiopathic leukoplakia
Leukoplakia is an adaptive response of tissue. The mucosa is trying to adapt to the noxious stimuli like mechanical, chemical or galvanic stimuli by undergoing hyperkeratinization and causing epithelial hyperplasia. So, it is assumed as a negative diagnostic state.
Etiologic factors:
1. Tobacco: Smoking, chewing or reverse smoking
2. Alcohol: Synergistic effects
3. Candidiasis
4. Dietary deficiency: Vitamin A, B12, C, Folic acid.
5. Viral infections: HPV 16 and 18
6. Hormonal imbalance
7. Chronic irritation: By ill-defined dentures, sharp cuspal edges of teeth and hot or spicy foods.
Clinical Features:
Prevalence: 2.6 % globally
Age: Onset - 30 years, Peak - above 60 years
Sex: M:F = 2.5:1
Site: Buccal mucosa (most common), alveolar ridge, tongue, lips, soft and hard palate floor of mouth, gingiva
Clinical Presentations:

1. Solitary or multiple white patches over mucosa
2. Lesion can be thick, fissured, indurated or papillomatous
3. Size may vary from few mm to large diffused lesion
4. Color may be greyish white or yellowish white
5. Can't be removed by scraping
6. Pumice like surface
7. Ebbing tide pattern if involves floor of mouth
8. Symptoms may be:
a. Pain
b. burning sensation
c. feeling of thickness
Classification:
A) Clinical Classification:
1. Homogenous Leukoplakia: Lesions that are uniformly white.
a. Smooth
b. Indurated
c. Ulcerated
2. Non-homogenous: lesions that are partly white and partly red.
a. Nodular
b. Speckled
c. Verrucous
B) Modified Classification: Presented by Van Der Wal
L denotes size:
L1 - Size of leukoplakia < 2 cm
L2 - Size of leukoplakia 2 to 4 cm
L3 - Size of leukoplakia > 4 cm
L4 - Size not specified
P denotes pathology or dysplasia
P0 - No epithelial dysplasia
P1 - Distinct epithelial dysplasia
Px - Dysplasia not specified
OLEP staging system for leukoplakia:
Stage I - L1P0
Stage II - L2P0
Stage III - L3P0 or L1L2P1
Stage IV - L3P1
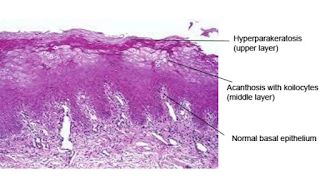 Histopathological features:
Histopathological features:Hallmarks:
1. Epithelial hyperplasia
2. Surface hyperkeratosis
3. Epithelial dysplasia (mild to severe)
Note:
- HPV associated dysplasia: Koilocytic dysplasia
- Lichenoid dysplasia: features resembling Lichen planus
- Tobacco: Chevron type keratinization
- C. Albicans: microabscess at superficial layer
Investigations for leukoplakia:
1. Histochemistry: a) Immunohistochemistry
b) Enzyme histochemistry
2. Exfoliate cytology
3. Cell proliferation study
4. Stereological technique
5. DNA histograms
6. In-vitro testing of living tissue
Malignant Transformation:
- 1 to 7% (homogenous)
- 4 to 15% (granular)
It will lead to Squamous cell carcinoma. Risk factors are:
1. Female
2. Long duration leukoplakia
3. Leukoplakia in nonsmokers
4. Presence of epithelial dysplasia
5. Size > 2cm
6. Location on tongue and floor of mouth
7. Nodular type
8. DNA aneuploidy
Treatment of leukoplakia:
1. Stoppage of all bad oral habits
2. Surgical excision of lesion or cryosurgery
3. Administration of heavy dose of Vitamin A
4. Photodynamic surgery
5. Co2 laser therapy
Differential diagnosis of leukoplakia:
1. Lichen planus
2. Candidiasis
3. Trichinal Keratosis
4. Verrucous carcinoma
5. Leukoedema
6. Syphilitic patches
7. Chemical burns
8. Discoid lupus erythematosus
Thank You for Visiting

No comments:
Post a Comment